Heart Failure
What is a Middle Ear Infection?
Ear is one of the most delicate sense organs. If it is not cared properly, it may cause several problems, including ear infection. Ear infection is a very common problem, diagnosed in infants and children. Even it is common in adults, now-a-days. The general term used for ear infection is “Otitis Media” or chronic ear infection. Very few people know about the symptoms, causes, and treatment of an ear infection. If we suffer with an ear pain, we always try to sort out a quick remedy to overcome it. Before going through the series of home remedies, let us understand the symptoms and causes of an ear infection.
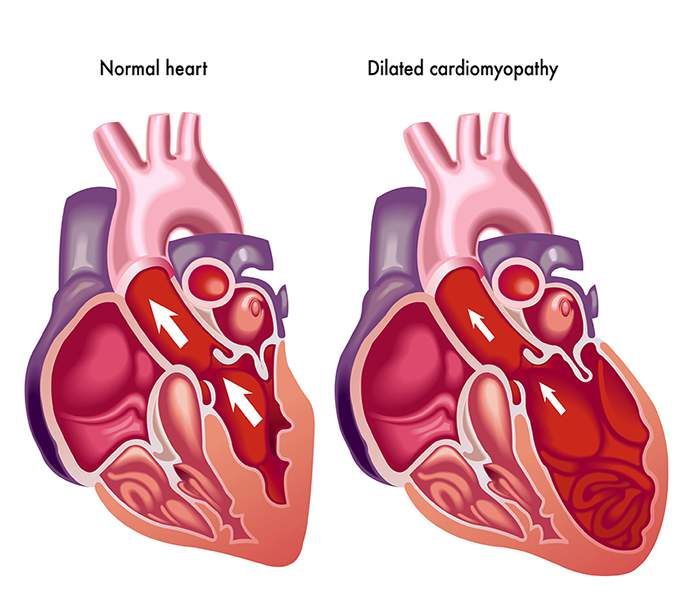
What Is Heart failure?
Heart failure is not as deadly as its name implies though it sound like the heart is no longer working at all and there is nothing that can be done. Actually, heart failure means that the heart is not pumping as well as it should be.
Your body depends on the heart's pumping action to deliver oxygen- and nutrient-rich blood to the body's cells. When the cells are nourished properly, the body can function normally.
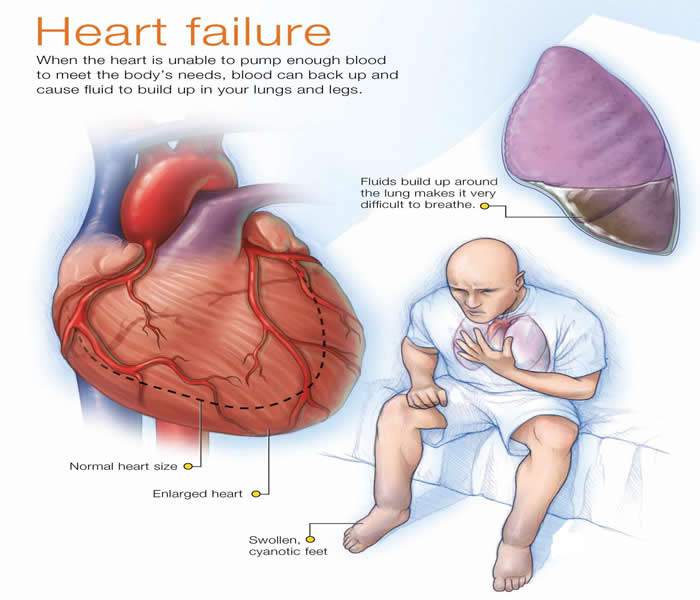
With heart failure, the weakened heart cannot supply the cells with enough blood. This result in fatigue and shortness of breath and some people have coughing. Everyday activities such as walking, climbing stairs or carrying groceries can become very difficult.
Heart failure means that the heart is unable to pump blood around the body properly. It usually occurs because the heart has become too weak or stiff.
Type of heart failure |
Description |
|
Fluid may back up in your lungs, causing shortness of breath. |
|
Fluid may back up into your abdomen, legs and feet, causing swelling. |
|
The left ventricle can't contract vigorously, indicating a pumping problem. |
|
The left ventricle can't relax or fill fully, indicating a filling problem. |
Causes of Heart failure
Heart failure often develops after other conditions have damaged or weakened your heart. However, the heart doesn't need to be weakened to cause heart failure. It can also occur if the heart becomes too stiff.
In heart failure, the main pumping chambers of your heart (the ventricles) may become stiff and not fill properly between beats.
- Alcohol / drug abuse
- Congenital heart defects
- Coronary artery disease
- Diabetes
- Heart muscle disease or inflammation of the heart
- Heart valve disease
- High blood pressure
- Lung conditions
- Past heart attacks
Diabetes: Diabetes is a disease in which the body’s blood glucose (sugar) level is too high. The body normally breaks down food into glucose and then carries it to cells throughout the body. The cells use a hormone called insulin to turn the glucose into energy.
In diabetes, the body doesn’t make enough insulin or doesn’t use its insulin properly. Over time, high blood sugar levels can damage and weaken the heart muscle and the blood vessels around the heart, leading to heart failure.
High Blood Pressure: Blood pressure is the force of blood pushing against the walls of the arteries. If this pressure rises and stays high over time, it can weaken your heart and lead to plaque buildup.
Blood pressure is considered high if it stays at or above 140/90 mmHg over time. (The mmHg is millimeters of mercury—the units used to measure blood pressure.) If you have diabetes or chronic kidney disease, high blood pressure is defined as 130/80 mmHg or higher.
Heart valve disease: The valves of your heart keep blood flowing in the proper direction through the heart. A damaged valve — due to a heart defect, coronary artery disease or heart infection — forces your heart to work harder to keep blood flowing as it should.
Over time, this extra work can weaken your heart. Faulty heart valves, however, can be fixed or replaced if found in time.
Conditions that can trigger Heart failure include:
- Abnormal heart rhythm
- Aneamia
- Infection
- Kidney disease / poor kidney function
- Overactive thyroid gland
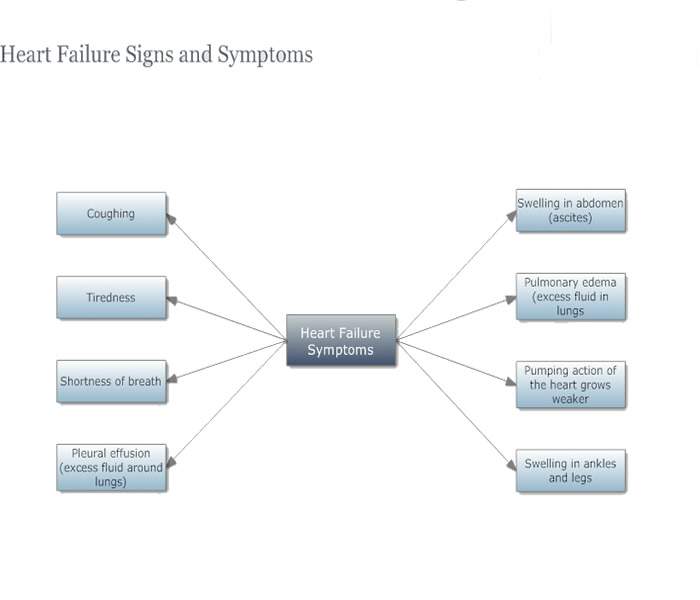
Symptoms/Signs of Heart failure
- Buildup of excess fluid in body tissues (edema)
- Confusion, impaired thinking
- Cough
- Everyday activities such as walking, climbing stairs or carrying groceries can become very difficult.
- Fatigue
- Increased heart rate
- Lack of appetite, nausea
- Persistent coughing or wheezing
- Shortness of breath (also called dyspnea)
- Tiredness, fatigue
How to diagnose Heart failure
How to Prevent Heart failure
Many things can put you at risk for these problems – one’s you can control, and others that you can’t. But the key takeaway is that with the right information, education and care, heart disease in women can be treated, prevented and even ended.
Studies show that healthy choices have resulted in 330 fewer women dying from heart disease per day. Here are a few lifestyle changes you should make:
- Do not smoke
- Eat healthy
- Get your blood pressure under control
- Lose weight
- Lower your cholesterol
- Know your family history
- Manage your blood sugar
- Stay active
Treatment for Heart failure
Heart failure caused by damage to the heart that has developed over time can't be cured. But it can be treated, quite often with strategies to improve symptoms.
Successful treatment depends on your willingness to get involved in managing this condition, whether you're the patient or a caregiver. You and your loved ones are an active part of the healthcare team.
Doctors usually treat heart failure with a combination of medications. Depending on your symptoms, you might take one or more medications, including:
Angiotensin-converting enzyme (ACE) inhibitors: These drugs help people with systolic heart failure live longer and feel better. ACE inhibitors are a type of vasodilator, a drug that widens blood vessels to lower blood pressure, improve blood flow and decrease the workload on the heart. Examples include enalapril (Vasotec), lisinopril (Zestril) and captopril (Capoten).
Angiotensin II receptor blockers: These drugs, which include losartan (Cozaar) and valsartan (Diovan), have many of the same benefits as ACE inhibitors. They may be an alternative for people who can't tolerate ACE inhibitors.
Beta blockers: This class of drugs not only slows your heart rate and reduces blood pressure but also limits or reverses some of the damage to your heart if you have systolic heart failure. Examples include carvedilol (Coreg), metoprolol (Lopressor) and bisoprolol (Zebeta).
These medicines reduce the risk of some abnormal heart rhythms and lessen your chance of dying unexpectedly. Beta blockers may reduce signs and symptoms of heart failure, improve heart function, and help you live longer.
Diuretics: Often called water pills, diuretics make you urinate more frequently and keep fluid from collecting in your body. Diuretics, such as furosemide (Lasix), also decrease fluid in your lungs so you can breathe more easily.
Because diuretics make your body lose potassium and magnesium, your doctor also may prescribe supplements of these minerals. If you're taking a diuretic, your doctor will likely monitor levels of potassium and magnesium in your blood through regular blood tests.
Aldosterone antagonists: These drugs include spironolactone (Aldactone) and eplerenone (Inspra). These are potassium-sparing diuretics, which also have additional properties that may help people with severe systolic heart failure live longer.
Unlike some other diuretics, spironolactone and eplerenone can raise the level of potassium in your blood to dangerous levels, so talk to your doctor if increased potassium is a concern, and learn if you need to modify your intake of food that's high in potassium.
Inotropes: These are intravenous medications used in people with severe heart failure in the hospital to improve heart pumping function and maintain blood pressure.
Digoxin (Lanoxin):This drug, also referred to as digitalis, increases the strength of your heart muscle contractions. It also tends to slow the heartbeat. Digoxin reduces heart failure symptoms in systolic heart failure. It may be more likely to be given to someone with a heart rhythm problem, such as atrial fibrillation.
You may need to take two or more medications to treat heart failure. Your doctor may prescribe other heart medications as well — such as nitrates for chest pain, a statin to lower cholesterol or blood-thinning medications to help prevent blood clots — along with heart failure medications.
You may be hospitalized if you have a flare-up of heart failure symptoms. While in the hospital, you may receive additional medications to help your heart pump better and relieve your symptoms. You may also receive supplemental oxygen through a mask or small tubes placed in your nose. If you have severe heart failure, you may need to use supplemental oxygen long term.
Medical Procedures and Surgery
As heart failure worsens, lifestyle changes and medicines may no longer control your symptoms. You may need a medical procedure or surgery.
In heart failure, the right and left sides of the heart may no longer contract at the same time. This disrupts the heart’s pumping. To correct this problem, your doctor might implant a cardiac resynchronization therapy device (a type of pacemaker) near your heart. This device helps both sides of your heart contract at the same time, which can decrease heart failure symptoms.
Some people who have heart failure have very rapid, irregular heartbeats. Without treatment, these heartbeats can cause sudden cardiac arrest. Your doctor might implant an implantable cardioverter defibrillator (ICD) near your heart to solve this problem. An ICD checks your heart rate and uses electrical pulses to correct irregular heart rhythms.
People who have severe heart failure symptoms at rest, despite other treatments, may need:
A mechanical heart pump, such as a left ventricular assist device, this device helps pump blood from the heart to the rest of the body. You may use a heart pump until you have surgery or as a long-term treatment.
Heart transplant: A heart transplant is an operation in which a person’s diseased heart is replaced with a healthy heart from a deceased donor. Heart transplants are done as a life-saving measure for end-stage heart failure when medical treatment and less drastic surgery have failed.
Heart failure Home Remedies/Home Cure
Making lifestyle changes can often help relieve signs and symptoms of heart failure and prevent the disease from worsening. These changes may be among the most important and beneficial you can make. Lifestyle changes your doctor may recommend include:
Stop smoking. Smoking damages your blood vessels, raises blood pressure, reduces the amount of oxygen in your blood and makes your heart beat faster.
If you smoke, ask your doctor to recommend a program to help you quit. You can't be considered for a heart transplant if you continue to smoke. Avoid secondhand smoke, too.
Discuss weight monitoring with your doctor. Discuss with your doctor how often you should weigh yourself. Ask your doctor how much weight gain you should notify him or her about. Weight gain may mean that you're retaining fluids and need a change in your treatment plan.
Check your legs, ankles and feet for swelling daily. Check for any changes in swelling in your legs, ankles or feet daily. Check with your doctor if the swelling worsens.
Eat a healthy diet. Aim to eat a diet that includes fruits and vegetables, whole grains, fat-free or low-fat dairy products, and lean proteins.
Restrict salt in your diet. Too much sodium contributes to water retention, which makes your heart work harder and causes shortness of breath and swollen legs, ankles and feet.
Check with your doctor for the sodium restriction recommended for you. Keep in mind that salt is already added to prepared foods, and be careful when using salt substitutes.
Maintain a healthy weight. If you're overweight, your dietitian will help you work toward your ideal weight. Even losing a small amount of weight can help.
Consider getting vaccinations. If you have heart failure, you may want to get influenza and pneumonia vaccinations. Ask your doctor about these vaccinations.
Limit fats and cholesterol. In addition to avoiding high-sodium foods, limit the amount of saturated fat, trans fat and cholesterol in your diet. A diet high in fat and cholesterol is a risk factor for coronary artery disease, which often underlies or contributes to heart failure.
Limit alcohol and fluids. Your doctor likely will recommend that you don't drink alcohol if you have heart failure, since it can interact with your medication, weaken your heart muscle and increase your risk of abnormal heart rhythms.
If you have severe heart failure, your doctor may also suggest you limit the amount of fluids you drink.
Be active. Moderate aerobic activity helps keep the rest of your body healthy and conditioned, reducing the demands on your heart muscle. Before you start exercising though, talk to your doctor about an exercise program that's right for you. Your doctor may suggest a walking program.
Check with your local hospital to see if it offers a cardiac rehabilitation program; if it does, talk to your doctor about enrolling in the program.
Reduce stress. When you're anxious or upset, your heart beats faster, you breathe more heavily and your blood pressure often goes up. This can make heart failure worse, since your heart is already having trouble meeting the body's demands.
Find ways to reduce stress in your life. To give your heart a rest, try napping or putting your feet up when possible. Spend time with friends and family to be social and help keep stress at bay.
Sleep easy. If you're having shortness of breath, especially at night, sleep with your head propped up using a pillow or a wedge. If you snore or have had other sleep problems, make sure you get tested for sleep apnea.
To improve your sleep at night, prop up your head with pillows. Also, discuss with your doctor changing the time for taking medications, especially diuretics. Taking diuretics earlier in the day may decrease the need to urinate as often during the night.
By Mayo Clinic
Complications of Heart failure
Heart failure occurs when the heart cannot adequately pump blood throughout the body. This can cause shortness of breath, dizziness, confusion, and the buildup of fluid in the body, causing swelling.
Heart Attack
A heart attack occurs when the coronary arteries narrow so much that they cut off blood supply to the heart. The heart cells begin to die as they are deprived of oxygen. Symptoms include shortness of breath and severe chest pain that may radiate to the back, jaw, or left arm.
Stroke
When the heart isn’t working effectively, blood clots are more likely to form in the blood vessels. A stroke occurs when one of these clots lodges in a blood vessel in the brain and cuts off blood flow. Stroke symptoms include:
- Numbness on one side of the body
- Confusion
- Trouble speaking
- Loss of balance or coordination
Pulmonary Embolism
A pulmonary embolism is similar to a stroke, but the blocked blood vessel is in the lungs instead of the brain. Symptoms include shortness of breath, chest pain on breathing, and bluish skin.
Cardiac Arrest
Cardiac arrest occurs when the heart suddenly stops beating. It’s usually caused by an electrical disturbance in the heart. Arrhythmias caused by heart disease can lead to cardiac arrest. This will lead to death if not treated immediately.
Peripheral Artery Disease (PAD)
The same narrowing that occurs in coronary artery disease can happen in the arteries that supply blood to the arms and legs. The main symptom of PAD is severe leg pain when walking.




