Depression
What Is Depression?
Depression is a common but serious mood disorder. It causes severe symptoms that affect how you feel, think, and handle daily activities, such as sleeping, eating, or working.
It is more than just a low mood – its a serious condition that affects your physical and mental health.
Depression is intense feelings of sadness and other symptoms, like losing interest in things you enjoy, may last for a while. Depression is a medical illness. It affects how you feel about yourself and makes life more difficult to manage from day to day.
It is a common and debilitating mood disorder that is affecting more and more people around the world. It is a serious illness caused by changes in brain chemistry.
Types of Depression
Some forms of depression are slightly different, or they may develop under unique circumstances, such as:
Persistent depressive disorder (also called dysthymia) is a depressed mood that lasts for at least two years. A person diagnosed with persistent depressive disorder may have episodes of major depression along with periods of less severe symptoms, but symptoms must last for two years to be considered persistent depressive disorder.
Perinatal depression is much more serious than the Persistent (relatively mild depressive and anxiety symptoms that typically clear within two weeks after delivery) that many women experience after giving birth. Women with perinatal depression experience full-blown major depression during pregnancy or after delivery (postpartum depression). The feelings of extreme sadness, anxiety, and exhaustion that accompany perinatal depression may make it difficult for these new mothers to complete daily care activities for themselves and/or for their babies.
Psychotic depression occurs when a person has severe depression plus some form of psychosis, such as having disturbing false fixed beliefs (delusions) or hearing or seeing upsetting things that others cannot hear or see (hallucinations). The psychotic symptoms typically have a depressive “theme,” such as delusions of guilt, poverty, or illness.
Seasonal affective disorder is characterized by the onset of depression during the winter months, when there is less natural sunlight. This depression generally lifts during spring and summer.
Winter depression, typically accompanied by social withdrawal, increased sleep, and weight gain, predictably returns every year in seasonal affective disorder.
Bipolar disorder is different from depression, but it is included in this list is because someone with bipolar disorder experiences episodes of extremely low moods that meet the criteria for major depression (called “bipolar depression”). But a person with bipolar disorder also experiences extreme high – euphoric or irritable – moods called “mania” or a less severe form called “hypomania.”
Classification of Depression
- Mild depression
- Mild to moderate depression
- Moderate to severe depression
Who is at risk?
Depression does not discriminate. Men and women of every age, educational level, and social and economic background suffer from depression.
Causes of Depression
Depression can be due to a number of factors including stresses which can range from mild to severe, combined with vulnerability or predisposition to depression that can result from biological, genetic or psychological factors.
Each type of depression is associated with different mixtures of causes. For psychotic or melancholic depression, physical and biological factors are relevant. In contrast, for non-melancholic depression, the role of personality and stressful life events are important.
Although scientists agree that depression is a brain disorder, the debate continues about exact causes. Many factors may contribute to the onset of depression, including genetic characteristics, changes in hormone levels, certain medical illnesses, stress, grief, or substance abuse. Any of these factors alone or in combination can bring about the specific changes in brain chemistry that lead to the many symptoms of depression, bipolar disorder and related conditions.
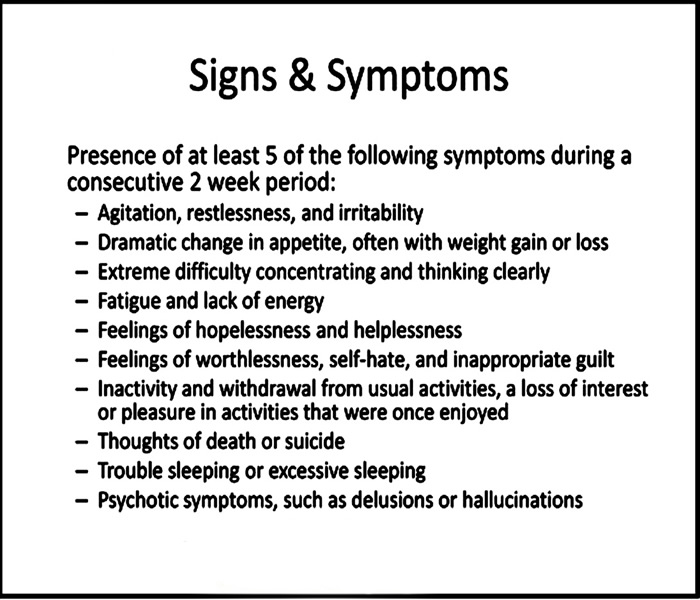
Symptoms/Signs of Depression
Behaviour
- Not going out anymore
- Not getting things done at work/school
- Not doing usual enjoyable activities
- Relying on alcohol and sedatives
- Unable to concentrate
- Withdrawing from close family and friends
Feelings
- Disappointed
- Guilty
- Frustrated
- Indecisive
- Irritable
- Lacking in confidence
- Overwhelmed
- Miserable
- Sad
- Unhappy
Physical
- Churning gut
- Headaches and muscle pains
- Loss or change of appetite
- Significant weight loss or gain
- Sleep problems
- Sick and run down
- Tired all the time
Thoughts
- I am a failure.
- It is my fault.
- Nothing good ever happens to me.
- I am worthless.
- Life is not worth living.
- People would be better off without me.
Note:
To be diagnosed with depression, the symptoms must be present for at least two weeks.
How to diagnose Depression
Your doctor can usually tell if you have depression by asking you specific questions and doing a physical exam. Your doctor may, however, ask for lab tests to rule out other diagnoses. Your doctor will likely do blood tests to check for medical conditions that may cause depressive symptoms.
How to Prevent Depression
- Avoid alcohol and drugs: Alcohol is a depressant that can alter your mood without you even realizing it. What’s more, those at risk for depression are also at greater risk of alcohol abuse and developing alcoholism. To be safe in the short and long term, just avoid it.
- Do not blame yourself
- Exercise regularly
- Get the right amount of sleep
- Eat a healthy diet
- Focus on having a positive attitude
- Join a support group
- Monitor your overall health
- Taking Care of Your Mind
- Think of what you’re grateful for every day
- Volunteer: Getting out of your head and into the zone of helping others helps keep you busy, your mind buzzing with positivity, and helps you feel good about yourself and the world around you. Volunteering cultivates a positive attitude and helps better the world. It is a win-win
- Work on your passions to find an outlet and to cultivate your self-esteem
- Regulate your blood sugar
Treatment for Depression
Three of the more common methods used in depression treatment include cognitive behavioral therapy, interpersonal therapy, and psychodynamic therapy. Often, a blended approach is used.
Mild depression:
Wait and see – if you're diagnosed with mild depression, your depression may improve by itself. In this case, you'll simply be seen again by your GP after two weeks to monitor your progress. This is known as watchful waiting.
Exercise: there is evidence that exercise may help depression and it is one of the main treatments if you have mild depression. Your GP may refer you to a qualified fitness trainer for an exercise scheme, or you can find out more about starting exercise here. Read more about exercise for depression.
Self-help groups: talking through your feelings can be helpful. You could talk either to a friend or relative, or you can ask your GP to suggest a local self-help group. Find out more about depression support groups. Your GP may also recommend self-help books and online cognitive behavioural therapy (CBT).
Mild to moderate depression
Talking therapy – if you have mild depression that isn't improving, or you have moderate depression, your GP may recommend a talking treatment (a type of psychotherapy). There are different types of talking therapy for depression, including cognitive behavioural therapy (CBT) and counselling. Your GP can refer you for talking treatment or in some parts of the country you might be able to refer yourself.
Moderate to severe depression
Antidepressants – antidepressants are tablets that treat the symptoms of depression. There are almost 30 different kinds of antidepressant. They have to be prescribed by a doctor, usually for depression that is moderate or severe.
Combination therapy – your GP may recommend that you take a course of antidepressants plus talking therapy, particularly if your depression is quite severe. A combination of an antidepressant and CBT usually works better than having just one of these treatments.
Mental health teams – if you have severe depression, you may be referred to a mental health team made up of psychologists, psychiatrists, specialist nurses and occupational therapists. These teams often provide intensive specialist talking treatments as well as prescribed medication.

Depression Home Remedies/Home Cure
1. Get enough sleep.
There’s nothing like tossing and turning all night to put you in a bad mood, but sleep disturbances may go further than that. According to researchers, disturbances in circadian rhythms have been linked to depression, and resynchronizing circadian rhythms using melatonin supplements or light therapy may actually have antidepressant effects.
Whether you’re dealing with major depression or just looking to boost your mood, improving your sleep hygiene is an important first step. Go to bed at the same time each day, turn off the screens a bit earlier than normal, and look into light therapy if your work schedule means you don’t get much sunlight.
2. Exercise.
You’ve probably heard this before, but listen up: Exercise is incredibly valuable, not only for general health, but for its mood-boosting effects, too. You don’t need to run a marathon to reap the benefits of exercise. In a recent study, researchers had depressed patients pedal a stationary bike, measuring their subjective symptoms and cortisol (stress hormone) levels before and afterwards. They found that after just 15 minutes of exercise, both the patients’ symptoms of depression and cortisol levels were significantly reduced.
3. Regulate your blood sugar.
Have you ever eaten a sugary snack, only to find yourself starving and miserable an hour later? What goes up must come down, and a blood sugar spike followed by a crash is a one-way ticket to a lousy mood. But according to one study, sugar may have a bigger role to play in depression than originally thought. Researchers analyzed data from six countries and found a highly significant correlation between sugar consumption and depression rates.
Whether you’re battling depression or just trying to avoid the afternoon crash, balancing your blood sugar is key. Make sure to eat regular meals and snacks, including a good source of protein at every one.
4. Eat healthy fats.
Are you getting enough fish in your diet? Researchers have found that eating omega-3 polyunsaturated fatty acids (like those found in salmon, trout and sardines) reduces symptoms of depression. Flaxseeds and walnuts are also great sources of omega-3s.
5. Find passion in life.
Even if you’re eating healthy, getting enough sleep and doing your exercise, nothing will boost your mood like having a sense of purpose. According to Blue Zones, people who have a sense of purpose live up to seven years longer than those who don’t.
Complications of Depression
- Alcohol or substance misuse
- Anxiety, panic disorder or social phobia
- Excess weight or obesity, which can lead to heart disease and diabetes
- Family conflicts, relationship difficulties, and work or school problems
- Premature death from other medical conditions
- Pain and physical illness
- Self-mutilation, such as cutting
- Social isolation
- Suicidal feelings, suicide attempts or suicide




