Epilepsy
What Is Epilepsy?Epilepsy is a common serious neurological condition where there is a tendency to have seizures that start in the brain. Epilepsy is usually only diagnosed after a person has had more than one seizure.
Epilepsy is a common brain disorder characterized by recurrent seizures.
Epilepsy is a condition that affects the brain. When someone has epilepsy, it means they have a tendency to have epileptic seizures.
Causes of Epilepsy
Causes of epilepsy vary by age of the person. Some people with no clear cause of epilepsy may have a genetic cause. But what is true for every age is that the cause is unknown for about half of everyone with epilepsy. While in some cases the list below could course it.
- Many without a clear cause of epilepsy may have a genetic form.
- Brain tumors
- Genetic conditions that result in brain injury, such as tuberous sclerosis
- Head injury
- Head injuries that occur during birth or from accidents during youth or adulthood
- Infections such as meningitis or encephalitis
- Low oxygen during birth
- Stroke
- Scar
- The brain not developing properly
NOTE: Epilepsy leads to seizures
Common causes of seizures by age:
In Newborns:
Brain malformations
Lack of oxygen during birth
Low levels of blood sugar, blood calcium and eletrolyte disturbances
Inborn errors of metabolism
Intracranial hemorrhage
Maternal drug use
In Infants and Children:
Fever (febrile seizures)
Brain tumor (rarely)
Infections
In Children:
Congenital conditions (Down's syndrome, tuberous sclerosis and neurofibromatosis)
Genetic factors
Head trauma
Progressive brain disease (rare)
In Adult:
Alzheimer's disease
Stroke
Trauma
Symptoms/Signs of Epilepsy
Most Common Symptoms of Epilepsy are:
- A staring spell
- Loss of consciousness or awareness
- Psychic symptoms
- Temporary confusion
- Uncontrollable jerking movements of the arms and legs
Motor signs include the following:
- Alternating contraction and relaxation of muscle groups
- Asymmetrical posturing of the limbs
- Eye movements and turning of the head to the same side
- Speech arrest, vocalization
- Seeing flashes of lights or colors
- Autonomic signs and symptoms include the following:
- Borborygmi (rumbling noises produced by gas in the intestines)
- Illusions
- Hallucinations
- Experiencing unpleasant odors and tastes
- Dizziness, lightheadedness
- Flushing
- Hearing humming, buzzing, hissing noises
- Incontinence
- Nausea, vomiting
- Piloerection (goose bumps)
- Pupillary dilation
- Sweating
- Tachycardia (rapid heart rate)
Psychic symptoms include the following:
- Detachment, depersonalization
- Dreamy state
- Time distortion
- Unprovoked emotion: fear, pleasure, displeasure, depression, anger, elation, eroticism
Loss of consciousness distinguishes complex partial seizures from simple partial seizures. While unconscious, the patient may have "vacant" or "frightened" look and may have signs and symptoms of a simple partial seizure. Automatisms may occur during unconsciousness.
There are five types of automatisms:
Alimentary: chewing, increased salivation, borborygmi (rumbling noises caused by gas in the intestines)
Ambulatory: wandering, running
Mimetic: facial expressions of fear, bewilderment, discomfort, tranquility, laughter, crying
Gestural: repetitive movements of the hands, fingers, sexual gestures
Verbal: repeated short phrases or swearing
Patients who have had complex partial seizures over a period of years may develop drop attacks. When this occurs, they lose postural tone and fall with the sudden onset of unconsciousness.
Symptoms of Tonic-Clonic (formerly called Grand Mal) Seizures
Generalized tonic-clonic seizures may begin as simple or complex partial seizures. They may begin with aura, but patients often do not remember this phase. The tonic phase consists of the following:
- Extension of arms, legs, and/or face
- Fall
- Fingers and jaw clenched
- Loss of consciousness
- Yell or "tonic cry"
Epilepsy is usually only diagnosed after a person has had more than one seizure.
Your doctor would ask about your past (Health history)
To diagnose your condition, your doctor will review your symptoms and medical history. Your doctor may order several tests to diagnose epilepsy and determine the cause of seizures.
Neurological examination: Your doctor may test your behavior, motor abilities, mental function and other areas to diagnose your condition and determine the type of epilepsy you may have.
Blood tests: Your doctor may take a blood sample to check for signs of infections, genetic conditions or other conditions that may be associated with seizures.
Your doctor may also suggest tests to detect brain abnormalities, such as:
- Illustration showing brain activity recorded by an EEG
- EEG brain activity
- CT scan illustration
- Pinpointing seizure location
Your doctor may give you instructions to do something that will cause seizures, such as getting little sleep prior to the test.
Computerized tomography (CT) scan: A CT scan uses X-rays to obtain cross-sectional images of your brain. CT scans can reveal abnormalities in your brain that might be causing your seizures, such as tumors, bleeding and cysts.
Magnetic resonance imaging (MRI): An MRI uses powerful magnets and radio waves to create a detailed view of your brain. Your doctor may be able to detect lesions or abnormalities in your brain that could be causing your seizures.
Functional MRI (fMRI): A functional MRI measures the changes in blood flow that occur when specific parts of your brain are working. Doctors may use an fMRI before surgery to identify the exact locations of critical functions, such as speech and movement, so that surgeons can avoid injuring those places while operating.
Positron emission tomography (PET): PET scans use a small amount of low-dose radioactive material that's injected into a vein to help visualize active areas of the brain and detect abnormalities.
Single-photon emission computerized tomography (SPECT): This type of test is used primarily if you've had an MRI and EEG that didn't pinpoint the location in your brain where the seizures are originating.
A SPECT test uses a small amount of low-dose radioactive material that's injected into a vein to create a detailed, 3-D map of the blood flow activity in your brain during seizures.
Doctors also may conduct a form of a SPECT test called subtraction ictal SPECT coregistered to magnetic resonance imaging (SISCOM), which may provide even more detailed results.
Neuropsychological tests: In these tests, doctors assess your thinking, memory and speech skills. The test results help doctors determine which areas of your brain are affected.
How to Prevent Epilepsy
Here are some tips that may help reduce your risk of having an epilepsy seizure:
- Avoid bright, flashing lights and other visual stimuli
- Avoid drugs and alcohol
- Avoid playing video games
- Get plenty of sleep each night — set a regular sleep schedule, and stick to it
- Eat a healthy diet
- Learn stress management and relaxation techniques
- Skip TV and computer time whenever possible
- Take all of your medications as prescribed by your doctor
- Deciding on which medicine to prescribe depends on such things as:
- Other medicines that you may take for other conditions
- Possible side-effects
- Whether you are pregnant or planning a pregnancy
- Your age
- Your type of epilepsy
Treatment for Epilepsy
The majority of epileptic seizures are controlled by medication, particularly anticonvulsant drugs. The type of treatment prescribed will depend on several factors, including the frequency and severity of the seizures and the person's age, overall health, and medical history.
Medications used to treat epilepsy include:
- Carbamazepine (Tegretol or Carbatrol)
- Diazepam (Valium) and similar tranquilizers, such as lorazepam (Ativan), Tranxene and clonazepam (Klonopin)
- Eslicarbazepine (Aptiom)
- Ethosuximide (Zarontin)
- Felbamate (Felbatol)
- Gabapentin (Neurontin)
- Lacosamide (Vimpat)
- Lamotrigine (Lamictal)
- Levetiracetam (Keppra)
- Oxcarbazepine (Oxteller XR or Trileptal)
- Perampanel (Fycompa)
- Phenobarbital
- Phenytoin (Dilantin or Phenytek)
- Pregabalin (Lyrica)
- Primidone( Mysoline)
- Tiagabine hydrochloride (Gabitril)
- Topiramate (Topamax)
- Valproate, valproic acid (Depakene, Depakote)
- Zonisamide (Zonegran)

Epilepsy Home Remedies/Home Cure
Some of the most commonly used herbs for epilepsy are:
- Burning Bush
- Groundsel
- Hydrocotyle
- Lily Of The Valley
- Mistletoe
- Mugwort
- Peony
- Scullcap
- Tree Of Heaven
- Valerian
- Folic Acid
- Vitamin B6
- Vitamin D
- Vitamin E
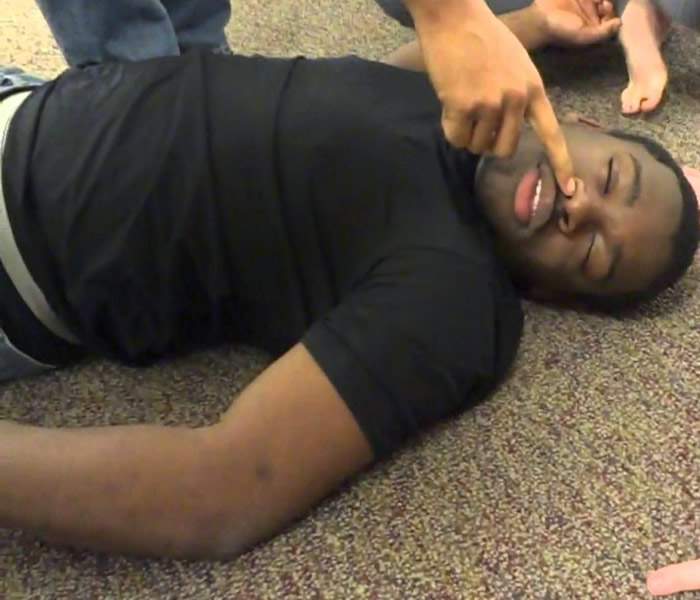
Injury: If an individual falls during a seizure, they may sustain a head injury. Drowning is a risk if the individual has a seizure while swimming or bathing.
Loss of consciousness and awareness: A seizure that causes either loss of awareness or control can be dangerous if the individual is driving a car or operating other equipment. Medications used to control seizures also can cause drowsiness, which may affect the individual's driving ability. Many states have licensing restrictions related to the individual's ability to control seizures.
Pregnancy: Seizures during pregnancy pose dangers to both mother and baby and certain anti-epileptic medications increase the risk of birth defects. A doctor will advise an individual with epilepsy who is considering becoming pregnant. Most women with epilepsy can become pregnant and have a healthy baby, but many need to adjust their medications and be carefully monitored throughout pregnancy.
Life-threatening complications: Life-threatening complications from epilepsy are uncommon, but do occur. Individuals who have severe, prolonged, or continuous seizures (status epilepticus) are at increased risk of permanent brain damage and death. Individuals with epilepsy, particularly those with poorly controlled epilepsy, also have a small risk of a condition called sudden unexplained death in epilepsy (SUDEP). The risk of SUDEP increases if the individual is having seizures at an early age, has frequent seizures that involve more than one area of the brain, or continues to have seizures despite treatment with medications.




