Staphylococcuss
What are Staphylococcuss?
What is Staphylococcuss
Staphylococcus is a group of bacteria that can cause a number of diseases as a result of infection of various tissues of the body. Staphylococcus is more familiarly known as staph (pronounced "staff"). Staph-related illness can range from mild and requiring no treatment to severe and potentially fatal.
Staphylococcus aureus is a type of bacteria. It stains Gram positive and is non-moving small round shaped or non-motile cocci. It is found in grape-like (staphylo-) clusters. This is why it is called Staphylococcus.
Causes of Staphylococcuss
Staph infections may cause disease due to direct infection or due to the production of toxins by the bacteria. Boils, impetigo, food poisoning, cellulitis, and toxic shock syndrome are all examples of diseases that can be caused by Staphylococcus.
Preventing staph infections
You can reduce your chances of developing staph infections by:
- Ensuring that food is both properly cooked and properly chilled – read more about preventing food poisoning
- Keeping your skin clean by having a bath or shower every day
- Keeping any cuts clean and covered
- Not sharing towels, washcloths, bed linen, toothbrushes and razors
- Washing your hands with soap and warm water regularly – particularly if you come into contact with someone who has a staph skin infection
If you experience repeated staph infections and you're found to carry the bacteria on your skin, your doctor may recommend using antibacterial shampoo and nasal cream to kill the bacteria and reduce the risk of further infections.
Symptoms/Signs of Staphylococcuss
Staph infections can range from minor skin problems to endocarditis, a life-threatening infection of the inner lining of your heart (endocardium). As a result, signs and symptoms of staph infections vary widely, depending on the location and severity of the infection.
Symptoms of Staph Infection
There are many different forms of staph infections, and each has different symptoms. The most common are:
Skin Infections: These staph-related conditions include boils, cellulitis, and impetigo.
Boils are hair follicles or oil glands that have become infected and are often filled with pus. The boil may be raised, swollen, red, and painful to the touch.
Boils most often occur in areas with a lot of friction, including under the arms, in the groin, and on the buttocks.
Cellulitis is an infection of the deeper layers of skin that causes your skin to swell, turn red, and become warm and tender.
Oozing sores (ulcers) may also develop. Cellulitis most often occurs in the lower legs and feet.
Impetigo is a highly contagious skin rash most commonly seen in children. An infected person will have blisters that ooze and crust over after a few days.
Food poisoning: Eating food that has been contaminated by staph bacteria is one of the most common causes of food poisoning.
Toxic shock syndrome: Also known as TSS, this potentially deadly condition results from toxins that are produced by some strains of staph bacteria.
TSS has been associated with the use of certain types of tampons, skin wounds, and surgery.
Septic Arthritis: Staph infection is a common cause of septic arthritis. The knees are most often affected, but the bacteria can target other joints including your ankle, hip, wrist, elbow, shoulder, or spine.
Bacteremia: Also known as blood poisoning, bacteremia is a more serious result of staph infection.
As the name suggests, it occurs when staph bacteria enter a person's bloodstream. Bacteremia can affect:
- Bones
- Brain
- Heart
- Kidneys
- Lungs
- Muscles
- Surgically implanted devices, such as artificial joints or cardiac pacemakers
Types of staph infections
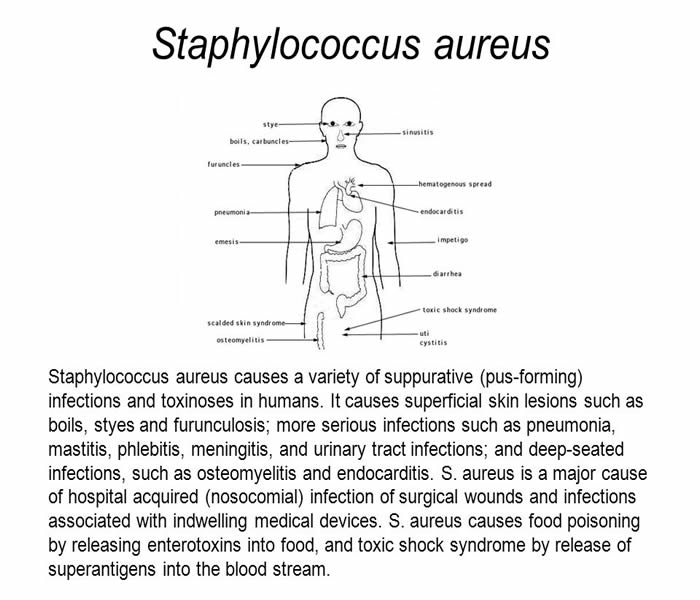
Staphylococcus aureus infections range from mild to life threatening. The bacteria tend to infect the skin (see Overview of Bacterial Skin Infections), often causing abscesses. However, the bacteria can travel through the bloodstream (called bacteremia) and infect almost any site in the body, particularly heart valves ( endocarditis) and bones ( osteomyelitis). The bacteria also tend to accumulate on medical devices in the body, such as artificial heart valves or joints, heart pacemakers, and catheters inserted through the skin into blood vessels.
Certain staphylococcal infections are more likely in certain situations:
Endocarditis: When people inject illegal drugs, have an infected blood vessel catheter, or have an artificial heart valve
Osteomyelitis: If Staphylococcus aureus spreads to the bone from infection in the bloodstream or from infection in adjacent soft tissue, as may occur in people with deep pressure sores or foot sores due to diabetes
Lung infection (pneumonia): When people have had influenza (particularly) or a bloodstream infection, when people are taking corticosteroids or drugs that suppress the immune system (immunosuppressants), or when they are hospitalized because they need tracheal intubation and mechanical ventilation (see Hospital-Acquired and Health Care–Associated Pneumonia)
There are many strains of Staphylococcus aureus. Some strains produce toxins that can cause the symptoms of staphylococcal food poisoning, toxic shock syndrome, and scalded skin syndrome.
Risk factors for staph infections
Certain conditions increase the risk of getting a staphylococcal infection:
- Chronic lung disorders (such as cystic fibrosis emphysema)
- Influenza
- Leukemia
- Tumors
A transplanted organ, an implanted medical device, or a catheter inserted into a blood vessel for a long time
- Burns
- Chronic skin disorders
- Diabetes mellitus
- Drugs, such as corticosteroids, drugs that suppress the immune system (immunosuppressants), cancer chemotherapy, or injected illegal drugs
- Radiation therapy
- Surgery
How to diagnose Staphylococcuss
Steps in diagnosis of S. aureus infections include:
Collection of specimens
This depends on the area of the body affected. For example, those with a skin infections or throat, nostrils and wound infections need to swabbed for pus and other discharge with the bacteria. Swabs consist of a sterile absorbent cotton tipped sticks. Those with a urinary tract infection need to provide a urine samples in sterile containers and those with a generalized blood infection need to provide blood samples. Blood samples are then transferred to blood culture bottle.
Identification of the bacteria
A small portion of the sample is swabbed onto a glass slide. This is then stained with Gram stain or dyes like crystal violet and basic fuschin and viewed under the microscope. S. aureus is Gram positive and stains blue or purple and appears as small round cocci or short chains and most commonly as grape-like clusters. Since S. aureus may be normally present on skin and mucous membranes, this test is not always confirmatory.
Confirmation of diagnosis
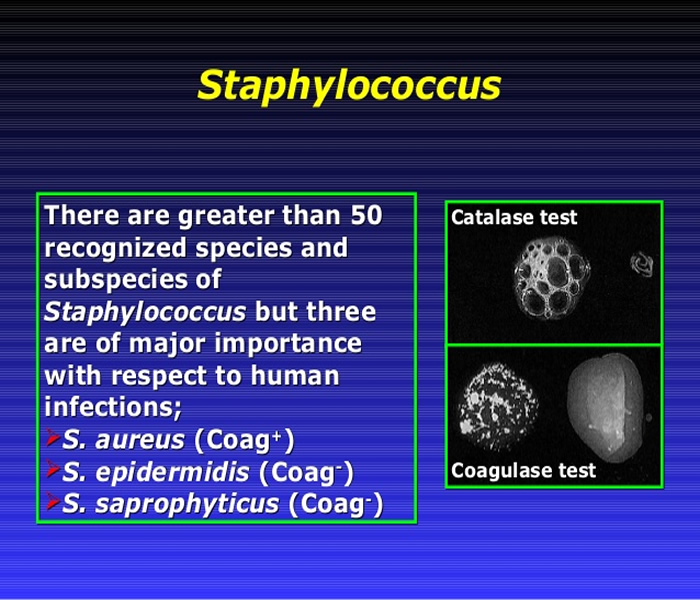
To confirm a diagnosis, the sample from the patient is placed onto a culture media. This could be a liquid or gel that provides sources of nutrition, carbon, energy and nitrogen for the bacteria to grow. For S. aureus, the medium used is suffused with blood and lactose. Also commonly used is the mannitol salt agar, which is a selective medium with 7–9% salt or sodium chloride that allows S. aureus to grow selectively. These media are placed on petri dishes and swabbed with the sample. The dishes are then incubated overnight at 37 degrees Celsius. After a set period of time the typical golden colonies of S. aureus are seen. These are then stained with Gram stain for confirmation and also undergo specific characteristic tests like the catalase test or the coagulase test for diagnosis.
Rapid diagnostic tests
These help in detection of the bacteria in real-time. These techniques include Real-time PCR and Quantitative PCR and are increasingly being employed in clinical laboratories.
Identification of toxins
This is important for more severe cases like toxic shock syndrome and food poisoning. Toxins produced by S. aureus, such as enterotoxins A to D and TSST-1 may be identified using agglutination tests. The tests are determined by clumping of the latex particles by the toxins present in the samples.
Antimicrobial assay studies
Many of the S. aureus strains are resistant to antibiotics. These assay studies help determine the specific susceptibility to antibiotics of the infected strain. Antibiotics like penicillin, amoxicillin, methicillin, first-generation cephalosporins, bactrim and vancomycin are commonly tested.
How to Prevent Staphylococcuss
- Avoid shared athletic equipment: Athletes are at a high risk for developing a staph infection because of the amount of bacteria that can be transferred through a piece of equipment. Avoid any loaner equipment like helmets, gloves, shoes or pads. If loaner equipment must be used, make sure it is sprayed and wiped down with disinfectant spray and wipes.
- Drink plenty of water: Try to drink anywhere between eight to ten glasses of water each day to help flush out bacteria from your body. Consuming more water each day also has many other health benefits.
- Hand sanitizer: Always carry hand sanitizer whenever possible. Keep it in your purse, your school bag, briefcase or in your car. Hand sanitizer is very useful when soap and water aren't available. You'll often see hand sanitizer dispensers in public areas like the gym or the mall; don't be afraid to use them!
- Do not share personal items: Soap, razors, ointments and towels being shared with others puts you at a greater risk of developing a staph infection. If you loan a towel to a friend who has a staph infection, and some of the fluids or pus from the wound wipe onto your towel, it becomes contaminated. If you use the towel again before washing it, and it touches a wound of your own, it's highly likely that you'll develop a staph infection as well.
- Disinfect areas that can easily be contaminated: Lockers, gym and athletic equipment, and bathrooms are areas that are filled with germs. Use disinfectant cleaners, sprays and wipes as often as possible and be mindful of the bacteria in such areas. If you plan on using a public shower, like in a gym locker room, make sure you wear slippers or some other type of cover for your feet.
- Keep away from other people's wounds: Avoid cuts and wounds on other individuals, especially if they are infected by Staph. The infection can be very contagious and can easily spread if you come in contact with the wound, or any liquid or pus from the wound.
- Properly treat your own wounds: Make sure any cuts or wounds on your body are kept clean and bandaged properly until they are fully healed. Walking around with an open wound is an invitation for Staph bacteria to enter the wound and infect it. This can either occur from contact with someone with staph infection, or a contaminated object or surface.
- Visit the doctor: Don't be afraid of paying a visit to the doctor if you feel there is a possibility you have a staph infection. Do not try to drain the liquid from a sore or boil yourself. If you notice that staph infections are being spread from one family member to another, notify your physician immediately.
- Wash your hands: Staph infections are one of the main reasons why it is so important to frequently wash your hands. Use hot water and soap, and make sure you do a thorough job. A quick splash of water does not equate to clean hands.
- Wash anything that has a higher possibility of carrying Staph bacteria immediately: Gym clothes, athletic apparel and clothing used in a hospital setting should be washed with hot water as soon as possible. This reduces the risk of developing a staph infection due to contaminated clothing.

Treatment for Staphylococcuss
Antibiotics commonly prescribed to treat staph infections include certain cephalosporins, nafcillin or related antibiotics, sulfa drugs or vancomycin. Vancomycin increasingly is required to treat serious staph infections because so many strains of staph bacteria have become resistant to other traditional medicines.
Antibiotic resistance of S. aureus
S. aureus strains may become resistant to penicillin by producing enzymes like penicillinase that destroys the antibiotic. This is a form of β-lactamase which breaks down the β-lactam ring of the penicillin molecule. To overcome this molecules resistant to penicillinase have been developed. These include:
- Cloxacillin
- Dicloxacillin
- Flucloxacillin
- Methicillin
- Nafcillin
- Oxacillin
Staphylococcuss Home Remedies/Home Cure
- Apple Cider Vinegar
A mixture can be prepared by adding apple cider vinegar (1/4th cup) and honey (4 – 5 teaspoons) in water (2 cups) and consumed 2 to 3 times in a day to treat staph infection.An individual can create a solution by mixing apple cider vinegar with baking soda and apply this solution with the help of a cotton swab on the affected area to deal with the problem of staph infection. - Basil
An individual can apply a juice extracted from fresh basil leaves on the affected area to treat various symptoms associated with staph infection. Basil oil can also be directly applied on the affected area to obtain the desired results. Regular intake of tea prepared by boiling basil leaves in water is also recommended. - Eucalyptus Oil : You can apply eucalyptus oil in combination with tea tree oil, lavender oil, rosemary oil, or oregano oil, in small quantities. This will provide a soothing relief to the boils, caused by a MRSA infection.
- Echinacea : Apply a cream, containing 15% of Echinacea, on the MRSA infection in order to get rid of it quickly. Echinacea is a useful herb that rapidly heals the infection while cleaning out the harmful bacteria from the area.
- Lapachol : Make lapachol tea by boiling it in a cup of water for about 10-15 minutes. Drink it at least 2-8 times a day. Lapachol is an effective herb, which helps in healing a MRSA infection.
- Thyme : Thyme oil can also be used as a natural treatment for MRSA. It should be taken internally as it is quite irritating to the skin.
- Goldenseal
Goldenseal has antibacterial properties. A solution can be created by mixing goldenseal powder in water and used for washing the affected area several times in a day to treat various symptoms associated with staph infection. - Garlic
An individual can apply crushed garlic cloves on the affected area to deal with staph infection. Garlic oil can also be directly applied on the affected area to obtain effective results. - Ginger
An individual can apply a paste created by mixing the ginger powder and salt in manuka honey on the affected area to reduce the staph infection. - Oregano Oil
You can use oregano oil for treating staph infection due to its antibiotic properties. Several chemical components in oregano oil help in reducing infection as effectively as traditional antibiotics. - According to a 2007 study published in the Journal of Medical Microbiology, researchers found there was a positive effect of oregano essential oil on staphylococcus aureus and staphylococcus epidermidis strains.
Dilute 8 to 10 drops of oregano oil in 2 tablespoons of olive oil or any other carrier oil. Apply it on the affected area and leave it on for a few hours before washing it off. Reapply several times a day.
Mix 5 drops of oregano oil in a glass of water or fruit juice. Drink it twice daily for a week.Note: Pregnant women should avoid intake of oregano oil.Applying oregano oil on the affected area multiple times in a day can help in curing the inflammation and pain resulting from staph infection
Turmeric
An individual can create a tonic by boiling turmeric powder (4 teaspoons), black pepper powder (1 teaspoon), coconut oil (1 teaspoon) and lemon juice (1 teaspoon) in water and consume this tonic several times in a day to cure staph infection. Turmeric powder can also be applied on the affected area to reduce the staph infection.Complications of Staphylococcuss
If staph bacteria invade your bloodstream, you may develop a type of infection that affects your entire body. Called sepsis, this infection can lead to septic shock — a life-threatening episode with extremely low blood pressure.




